Abstract
Introduction: High-dose post transplant cyclophosphamide (PTCY) effectively prevents graft-versus-host disease (GVHD) after unmanipulated HLA-haploidentical hematopoietic stem cell transplant (HSCT) and offer low rates of GVHD in the setting of HLA identical transplant. The objective of our study was to compare the outcomes of haplo vs HLA identical HSCT in patients undergoing HSCT for acute myeloid leukemia (AML) using PTCY.
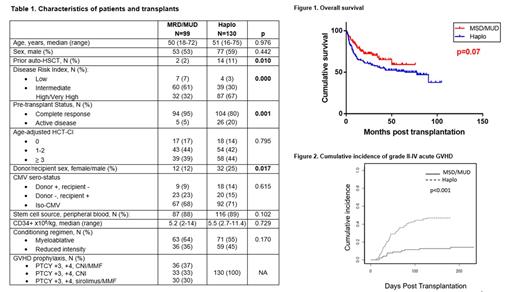
Patients and methods: We conducted a retrospective study of 229 patients undergoing a first HSCT for AML using PTCY, 130 from an haploidentical donor between 2013 and 2018 (median follow up 62.5 months) and 99 from a matched sibling (MSD) (n=38) or unrelated donor (MUD) (n=61) (median follow up 27 months) between 2013 and 2019, in 20 centers in Spain. Last update of the cohort was performed in March 2021.
Results: Baseline characteristics are summarized in Table 1. There were more patients with active disease at transplant (5% MSD/MUD vs. 20% haplo, p=0.001), high/very high DRI (32% vs. 67%, p=0.000) and prior autologous HSCT (2% vs. 11%, p=0.010) in the haplo group. Mobilized peripheral blood stem cells was the most frequent stem cell source in both groups. Most patients received myeloablative conditioning (55% vs. 64%, p=0.170). All Patients in the haplo group received PTCY days +3+4 followed by a calcineurin inhibitor (CNI) and MMF from +5. In the MSD/MUD group, 37% received both CNI+MMF, 33% only CNI and 30% PTCY with sirolimus+MMF (this group included only MUD donors). None of the patients received ATG. Cumulative incidence of neutrophil recovery at day 28 was 97% in both groups, with a median of 16 and 17 days respectively (p=0.948). Both 2-year overall survival (OS) (72% vs. 62%, p=0.07) and event-free survival (EFS) (70% vs. 54%, p=0.055) were higher in the MSD/MUD group, but the difference was not statistically significant (Figure 1). Multivariate analysis only identified age and pre-transplant status as independent risk factors for OS, and pre-transplant status for EFS. No differences were found in the cumulative incidence of relapse at 2 years (19% vs. 25%, p=0.13) and non-relapse mortality (14% vs. 19%, p=0.145). Cumulative incidence of grade II-IV acute GVHD was lower in MSD/MUD (14% vs. 47%, p=0.000, Figure 2), while III-IV aGVHD was similar (4% vs. 9%, p=0.14). Cumulative incidence of chronic GVHD and moderate-severe cGVHD at 2 years was similar for both groups (42% vs. 33% (p=0.051); 22% vs. 19% (p=0.28)). No differences were found in GRFS (48% vs. 46% (p=0.506)). Most frequent cause of death in the early post-transplant period was non-GVHD related infection in both groups.
Conclusions: in our experience, PTCY as GVHD prophylaxis in both MSD/MUD and Haplo transplant in AML using mostly PBSC effectively prevents GVHD and offers similar NRM, relapse and survival rates. Poor control of the disease before transplant was the only factor affecting OS and EFS in this setting. Prospective studies are needed to confirm our results.
Bailen: Pfizer, Kite-Gilead, Gilead: Honoraria. Guerreiro: Novartis, Gilead: Consultancy, Honoraria. Oarbeascoa: Gilead: Honoraria, Speakers Bureau. Kwon: Novartis, Celgene, Gilead, Pfizer: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal